Cardiovascular disease (CVD), one of the leading causes of death worldwide, is a broad category of ailments that are generally associated with the primary and accessory organs of the cardiovascular system. This system’s critical role is to deliver oxygen, nutrients, hormones, and other chemicals to the tissues of the body and to remove carbon dioxide and waste from those tissues.
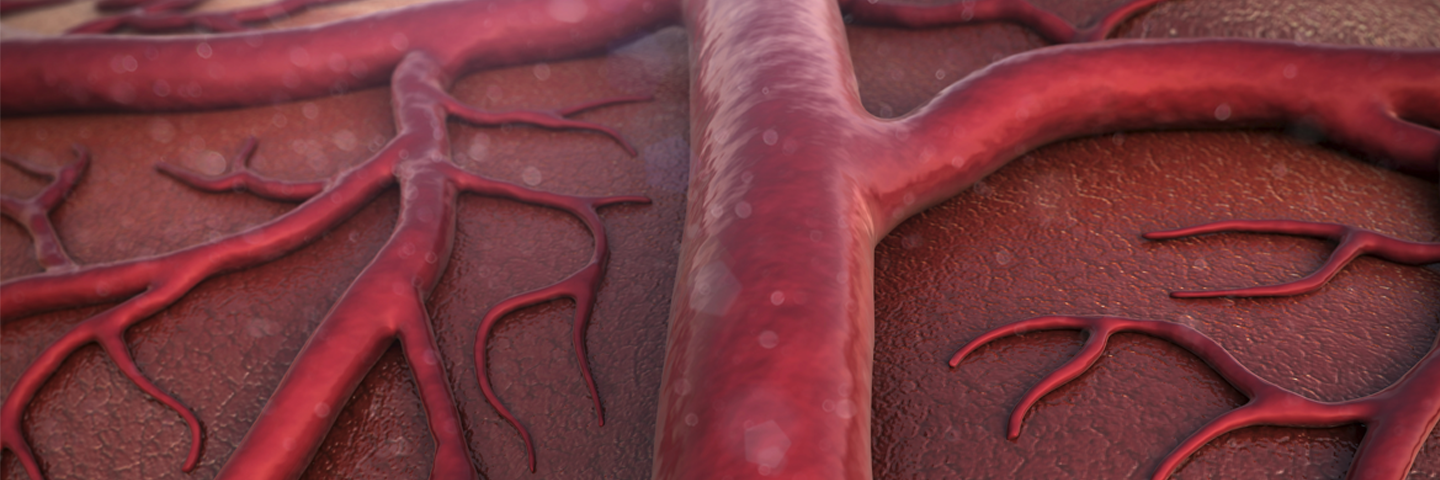
The primary organs of the cardiovascular system include the heart and blood vessels. Most of the anatomical structures that are related to the cardiovascular system display a common tissue organization. The innermost structure of the heart and blood vessels is a single layer of endothelial cells known as the tunica intima. These cells provide a smooth surface for blood flow and secrete factors that can locally or globally influence blood pressure.
Just superficial to the tunica is the tunica media, which is made up of smooth muscle cells. This tissue contracts or dilates in response to stretch or to cues from the endothelium. The outermost layer, the tunica adventitia (also known as the tunica externa), is made up of collagen and elastic fibers and serves to stabilize and anchor blood vessels. Capillaries, the smallest type of blood vessel, are composed of an endothelial layer and a basal membrane, while the heart, the aorta, arteries, arterioles, venules, and veins display all three layers of vascular tissue. Flow through this system is achieved via the contraction and relaxation cycle of the heart. In addition, many mechanisms exist to ensure that consistent perfusion of blood is sustained throughout the body, including local regulation, neural stimulation, endocrine modulation, and renal excretion.
Cardiovascular Diseases
Cardiovascular diseases include, but are not limited to:
|
|
Some of the most interesting areas of research around CVD include local blood pressure regulation, the renin – angiotensin – aldosterone system, and inflammation-associated CVD.
Angiogenesis
While the formation of new blood vessels is a normal part of development, growth, and repair, it also plays a role in diseases like cancer. Tumors need nutrients and oxygen to grow and spread, so they secrete vascular growth factors to stimulate angiogenesis to cause excessive blood vessels to grow into the tumor. To tackle this issue, clinicians have turned toward angiogenesis inhibitors to treat certain cancers.
Learn More
Cell Culture Fundamentals
Our cell culture experts share their techniques for successful culture and offer advice on process and products.
Learn MoreLocal Blood Pressure Regulation
As chronic vasoconstriction is associated with the development of hypertension, one major area of research over the years has been the identification of vasodilators and vasoconstrictors. These agents act on the smooth muscle cells of the tunica media, which control the diameter of the blood vessel’s lumen and thus blood flow. Vasodilation opens the lumen of the blood vessel, allowing more fluid through and reducing blood pressure. Some endogenous vasodilators include histamine, epinephrine (adrenaline), prostacyclin, prostaglandin D2 and E2, nitric oxide (NOS), bradykinin, and substance P. By contrast, vasoconstriction reduces the diameter of the blood vessel, resulting in increased blood pressure. Endogenous vasoconstrictors include mechanical stretch, endothelin 1, angiotensin II (Ang II), antidiuretic hormone, and ATP.
Hypertension and the Renin – Angiotensin – Aldosterone System
Another major area of research around cardiovascular disease is the renin – angiotensin – aldosterone system renin – angiotensin – aldosterone system. In this multi-organ system of blood volume control, the juxtaglomerular (JG) cells in the kidney release the enzyme renin in response to stimuli such as low arterial pressure or decreased sodium and chloride ion concentrations (sensed by the adjacent macula densa cells). Renin catalyzes the circulating hormone angiotensinogen to the weakly bioactive angiotensin I. Upon circulation through the vascular system (especially the lung vasculature), Angiotensin I is converted to the potently bioactive Ang II by angiotensin converting enzyme (ACE). Ang II has pleiotropic effects, including constriction of arterioles and release of antidiuretic hormone. In the third node of renin – angiotensin – aldosterone system, Ang II stimulates aldosterone secretion via binding with the g protein-coupled AT1 receptor of adrenal glomerulosa cells. Aldosterone, in turn, binds to steroid hormone receptors in renal epithelial cells in the kidney, inducing the cells to synthesize sodium potassium antiport transporters and sodium channels to facilitate the reabsorption of water from filtrate. The result of this renal reabsorption of water is an increase in blood volume, which in turn contributes to an increase in blood pressure. The renin – angiotensin – aldosterone system can be perturbed when other disease states manifest, such as adrenal carcinoma and kidney damage, bringing about hypertension and contributing to congestive heart failure. Inhibition of this pathway through ACE inhibitors, Ang II receptor blockers, and aldosterone receptor inhibitors can reduce blood pressure and improve long term survival for some CVD patients.
Inflammation and CVD
Inflammation has long been a central area of interest for researchers studying cardiovascular disease. For example, sustained levels of inflammation have been may cause damage to components of the cardiovascular system. In addition, inflammation may be mediated by atherosclerosis, or a buildup of cholesterol-containing plaques on the tunica intima that lines the lumen of blood vessels. This buildup draws monocytes, which are then stimulated to differentiate into a specific type of macrophage known as foam cells. These foam cells can then promote further plaque formation and inflammation. Eventually, the plaque may break off the lumen wall and block blood flow at some downstream location, causing heart attack and stroke.
By contrast, inflammation can affect the inner lining and valves of the heart. This condition, also known as endocarditis, is caused by an overgrowth of bacteria. For example, Streptococcus gordonii, a bacterial strain that normally lives on teeth, may enter the blood stream through bleeding gums and then lodge in the heart. S gordonii express a fibrinogen mimic that activate platelets, which clump around the bacteria. The clumps of platelets may eventually block blood supply to the heart or brain, or cause additional inflammation that results in cardiac damage, leading to rhythm irregularities or heart failure.
To address researchers’ need for highly characterized and authenticated models for CVD, ATCC offers an array of primary cells, hTERT-immortalized primary cells, and toxicity testing resources. Browse the resources and products below for more information.
iPSC-derived Primary Cells in Toxicological Assays
iPSC-derived primary cells lend the ability to run large toxicity studies and drug screens with highly biologically relevant cells.
Learn more
Primary Immune Cells
ATCC has the primary immune cells, including peripheral blood mononuclear cells (PBMCs), you need to design and test cell-based assays and treatments as part of your research and development. A typical vial of PBMCs includes progenitor populations such as CD14+ monocytes and lymphocytes such as cluster of differentiation (CD) 19+ B cells, CD4+ helper T cells, CD8+ cytotoxic T cells, and CD56+ natural killer (NK) cells.
Learn More